Health Cabinet Secretary Aden Duale on Thursday launched Kenya’s National Cervical Cancer Elimination Plan 2026–2030.
The event comes during the national symposium held as part of Kenya Cancer Awareness Month, under the theme “Accelerating Cervical Cancer Elimination: Strong Systems and Community Action for Every Girl and Every Woman.”
According to the Ministry of Health, Kenya records about 5,845 new cervical cancer cases each year, and of those cases, approximately 3,591 women die annually from cervical cancer.
Cervical cancer contributes about 12.2% of all cancer deaths in Kenya, highlighting its position as a leading cause of cancer-related mortality nationally.
The newly launched action plan seeks to reverse this trend by strengthening prevention, early detection, treatment and long-term follow-up.
At the core of the plan is Kenya’s commitment to the global 90–70–90 targets set by the World Health Organization (WHO). These targets aim to ensure that 90 per cent of girls are fully vaccinated against the Human Papillomavirus (HPV) by age 15, 70 per cent of women are screened for cervical cancer at least twice in their lifetime, and 90 per cent of women diagnosed receive timely and effective treatment.
Speaking during the launch, CS Duale said the government has already begun implementing key reforms to accelerate progress.
Among them is Kenya’s transition to a single-dose HPV vaccination schedule, a move expected to increase coverage by reducing logistical and financial barriers.
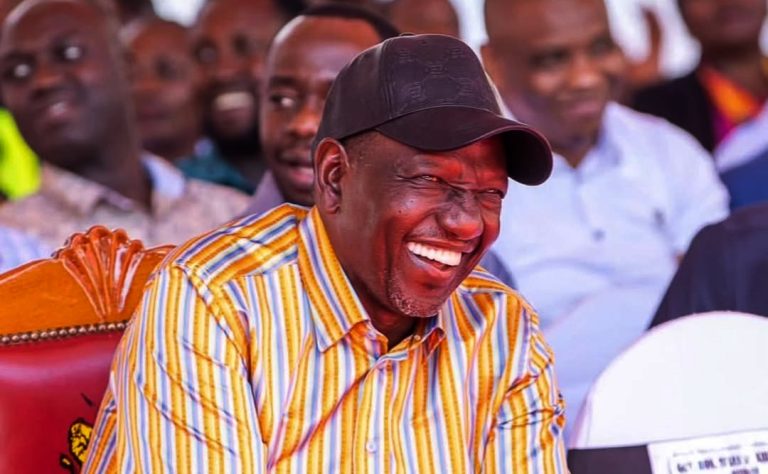
 Aden Duale speaking during the launch of Cervical Cancer elimination plan 2026-2030.
Aden Duale speaking during the launch of Cervical Cancer elimination plan 2026-2030.The Ministry of Health is also expanding HPV DNA testing and introducing self-sampling, allowing women to collect samples themselves, an approach seen as critical in improving screening uptake, especially in hard-to-reach and underserved communities across all 47 counties.
“We are strengthening referral systems, expanding cancer treatment infrastructure, and investing in a skilled health workforce,” Duale said, adding that health financing reforms under the Social Health Authority are intended to make cancer care more affordable and equitable.
In a move aimed at protecting patients, the Cabinet Secretary also announced the rollout of mandatory service charters in both public and private health facilities.
The charters will clearly display government-supported services, helping curb overcharging and improve transparency in healthcare delivery.
The symposium featured emotional testimonies from cervical cancer survivors, whose experiences highlighted the human cost of delayed diagnosis and treatment, as well as the life-saving impact of early screening and care.
With the plan, Kenya joins a growing number of countries working towards eliminating cervical cancer as a public health threat offering renewed hope that no woman or girl should die from a disease that is largely preventable.
by TIMON OTIENO